- 0share
- Follow
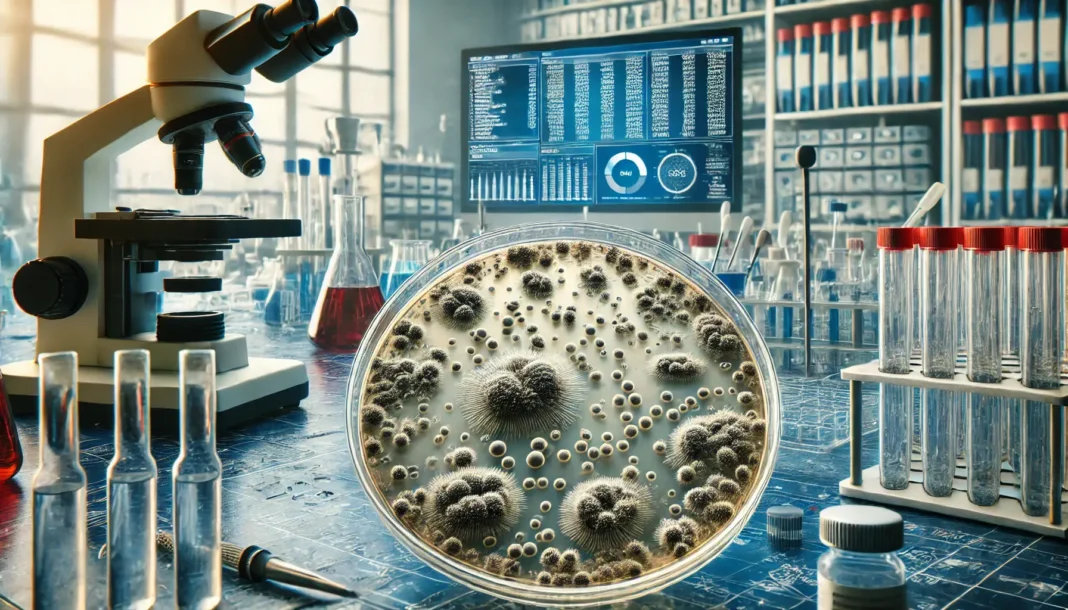
Researchers from the University of Sheffield and the University of Manchester have made a groundbreaking discovery regarding the rapid evolution of antibiotic resistance in Clostridioides difficile (C. diff), a notorious hospital superbug. The findings reveal how quickly C. diff can develop resistance to vancomycin, the frontline drug used in the UK, highlighting the urgency for better monitoring and new treatment strategies.
C. diff is a type of bacteria that commonly affects individuals who have recently taken antibiotics. Identified by the World Health Organisation (WHO) as one of the top global public health threats, C. diff is responsible for approximately 2,000 deaths annually in the UK alone. The bacteria can cause severe infections, particularly in hospital settings, where it thrives due to the high use of antibiotics.
The Discovery of Rapid Resistance Development
The research team found that C. diff can evolve to tolerate 32 times the usual concentration of vancomycin within a mere two months. This rapid development of antibiotic resistance poses a critical challenge to healthcare providers, as vancomycin is one of the few effective treatments available against C. diff infections.
This resistance evolution is particularly alarming because vancomycin is widely relied upon in UK healthcare to treat C. diff infections. However, the study’s findings suggest that routine monitoring for resistance in clinical settings is insufficient. Without vigilant surveillance, resistance could emerge undetected, rendering this vital treatment option ineffective.
The Global Threat of Antimicrobial Resistance (AMR)
Antimicrobial resistance (AMR) is a growing concern worldwide, with the WHO identifying it as one of the most significant public health and development threats of our time. According to recent estimates, bacterial AMR was directly responsible for 1.27 million deaths globally in 2019 and contributed to 4.95 million deaths. The rapid emergence of vancomycin-resistant C. diff strains could exacerbate this already dire situation.
Jessica Buddle, a PhD student at the University of Sheffield and the lead author of the study, emphasized the importance of monitoring vancomycin resistance in UK hospitals. She noted that unchecked resistance could contribute to the high rate of relapsing infections among patients treated with vancomycin. Currently, up to 30% of patients experience a second infection within weeks of treatment, with the risk of further relapses increasing over time.
Implications for Healthcare Policy and Future Research
The study’s findings underscore the need for more research to inform healthcare policies and determine whether vancomycin remains the best treatment option for C. diff infections. Understanding the mechanisms of resistance development and simulating these conditions within the complex human gut ecosystem are crucial next steps.
Buddle stated, “Our ongoing work aims to understand the extent and mechanisms of resistance development, simulate these conditions within the complex human gut ecosystem, and collaborate with UK epidemiologists to identify potential resistance signatures in hospitals.” These efforts are vital in preventing a future where antibiotics are no longer effective against bacterial infections.
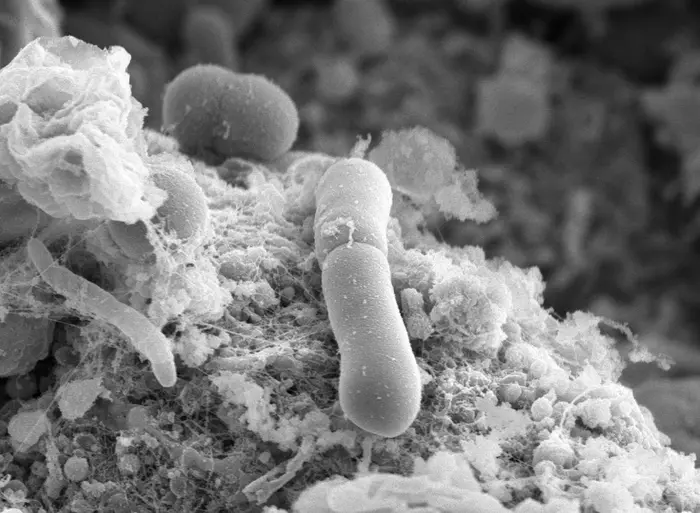
The Silver Lining: Reduced Fitness of Resistant Strains
Despite the concerning rapid evolution of resistance, the researchers found that the resistant C. diff strains exhibited reduced overall fitness. This reduced fitness could limit their clinical threat, as the strains may be less capable of causing severe disease. Additionally, these resistant strains often had defects in sporulation, a process essential for the bacteria’s transmission between individuals and survival on surfaces in hospitals.
Future research will explore the relationship between resistance and the ability of C. diff to cause severe disease. By leveraging this knowledge, researchers hope to improve the surveillance of emerging resistance in hospitals, ultimately safeguarding public health.
The discovery of C. diff’s rapid evolution of vancomycin resistance is a stark reminder of the challenges posed by antimicrobial resistance. With the potential to render one of the most critical treatments ineffective, this superbug’s adaptability underscores the need for enhanced monitoring, research, and policy changes. As the battle against antibiotic resistance continues, understanding the complex dynamics of resistance development will be key to preserving the effectiveness of existing treatments and preventing the resurgence of life-threatening infections.
Potential Links:
- University of Sheffield’s research on antimicrobial resistance (https://www.sheffield.ac.uk/research)
- WHO’s information on antimicrobial resistance (https://www.who.int/health-topics/antimicrobial-resistance)
- Information on C. diff from the CDC (https://www.cdc.gov/cdiff)
- 0share
- Follow