Researchers Develop Affordable Blood Test for Brain Cancer Detection
In a groundbreaking advancement, researchers at the University of Notre Dame have created an affordable blood test for brain cancer that can diagnose glioblastoma in less than an hour. Glioblastoma is a fast-growing and aggressive form of brain cancer, with patients typically surviving only 12-18 months after diagnosis. The new test offers hope for quicker and more accessible diagnosis, which could significantly impact patient outcomes.
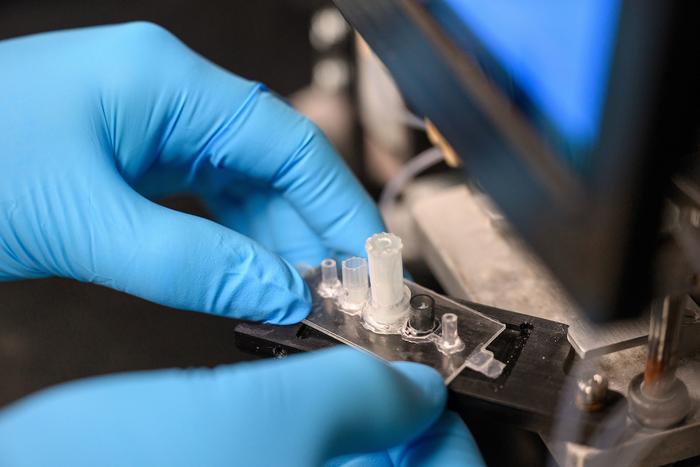
At the heart of this innovative diagnostic tool is a biochip that utilizes electrokinetic technology to detect specific biomarkers, notably active Epidermal Growth Factor Receptors (EGFRs). These receptors are often overexpressed in cancers like glioblastoma and are found in extracellular vesicles within blood samples.
Unique Nanoparticle Detection Technology
“Extracellular vesicles or exosomes are unique nanoparticles secreted by cells,” explained Hsueh-Chia Chang, the Bayer Professor of Chemical and Biomolecular Engineering at Notre Dame, who led the study. “They are significantly larger than molecules and have a weak charge. Our technology is designed to leverage these characteristics to enhance detection accuracy.”
The key challenge was to create a diagnostic device that could distinguish between active and inactive EGFRs with high sensitivity and selectivity. The biochip, roughly the size of a ballpoint pen tip, accomplishes this by using antibodies on the sensor to form multiple bonds with the extracellular vesicles. This approach dramatically improves the sensitivity and selectivity of the test.
A Cost-Effective Solution for Rapid Diagnosis
The biochip works by employing synthetic silica nanoparticles that “report” the presence of active EGFRs on the extracellular vesicles. These nanoparticles carry a high negative charge, and when active EGFRs are present, a detectable voltage shift occurs, confirming the presence of glioblastoma.
“Our electrokinetic sensor offers advantages over other diagnostic tools,” said Satyajyoti Senapati, a research associate professor at Notre Dame. “We can directly load blood samples without pretreatment to isolate extracellular vesicles because our sensor remains unaffected by other particles or molecules. This results in lower noise and greater sensitivity for disease detection compared to existing technologies.”
The diagnostic device comprises three main components: an automation interface, a portable prototype machine to administer the test, and the biochip. While each test requires a new biochip, the automation interface and machine are reusable. A single test takes less than an hour and requires only 100 microliters of blood. Additionally, the cost to produce each biochip is under $2, making this a highly cost-effective diagnostic solution.
Expanding Beyond Glioblastoma
Although initially developed for glioblastoma, the technology holds promise for detecting other types of diseases. “Our technique isn’t exclusive to glioblastoma. It was an ideal starting point due to the lack of early screening tests and the disease’s deadly nature,” said Chang. The research team is now exploring the potential of this technology in diagnosing other cancers, including pancreatic cancer, and conditions such as cardiovascular disease, dementia, and epilepsy.
The blood samples used for testing the device were provided by the Centre for Research in Brain Cancer at the Olivia Newton-John Cancer Research Institute in Melbourne, Australia.
Collaborative Effort with Far-Reaching Impact
This breakthrough was made possible through collaboration with multiple institutions. Besides Chang and Senapati, contributors include former Notre Dame postdocs Nalin Maniya and Sonu Kumar; researchers Jeffrey Franklin, James Higginbotham, and Robert Coffey from Vanderbilt University; and Andrew Scott and Hui Gan from the Olivia Newton-John Cancer Research Institute and La Trobe University. The study received funding from the National Institutes of Health Common Fund.
Chang and Senapati are affiliated with Notre Dame’s Berthiaume Institute for Precision Health, the Harper Cancer Research Institute, and NDnano, reflecting the interdisciplinary nature of this innovative research.