It’s no secret that antibiotic resistance is increasing around the world and for quite some time now researchers have been scrambling to find something that will overcome this dilemma. While various avenues have been explored, none have yet succeeded in achieving the required results. But, that could all be about to change.
New insight has been gathered from a study involving a type of multi-resistant bacterium called Pseudomonas aeruginosa, which is known to cause severe infections in humans. By observing this bacterium closer researchers have discovered that the strategy behind the evolution of its antibiotic resistance could be used to develop new and sustainable antibiotic therapies.
The first author of the study is Camilo Barbosa, a former postdoctoral student at the Kiel Evolution Center (KEC) of Kiel University in Germany. “Antibiotic resistance is one of the most serious threats to public health worldwide,” he says. “The World Health Organization warns of a post-antibiotic era in which infections can no longer be treated and could become one of the most frequent non-natural causes of death”.
With antibiotic resistance evolving so fast, the effect of antibiotic treatments also declines fast, and within a short space of time, become ineffective altogether. What this means is that new strategies need to be developed rapidly to counteract these detrimental effects. And in order to succeed, they need to take all the “relevant evolutionary processes into account,” explains Barbosa.
Collateral sensitivity occurs when resistance to bacteria evolves at the same time an increased sensitivity to a different drug is developed. “While a variety of distinct cases of collateral sensitivities have previously been described, it was still unclear whether they could be exploited for antibiotic treatment,” says Barbosa. “We tested one key requirement of this principle for medical implementation: stability of the evolutionary trade-off.”
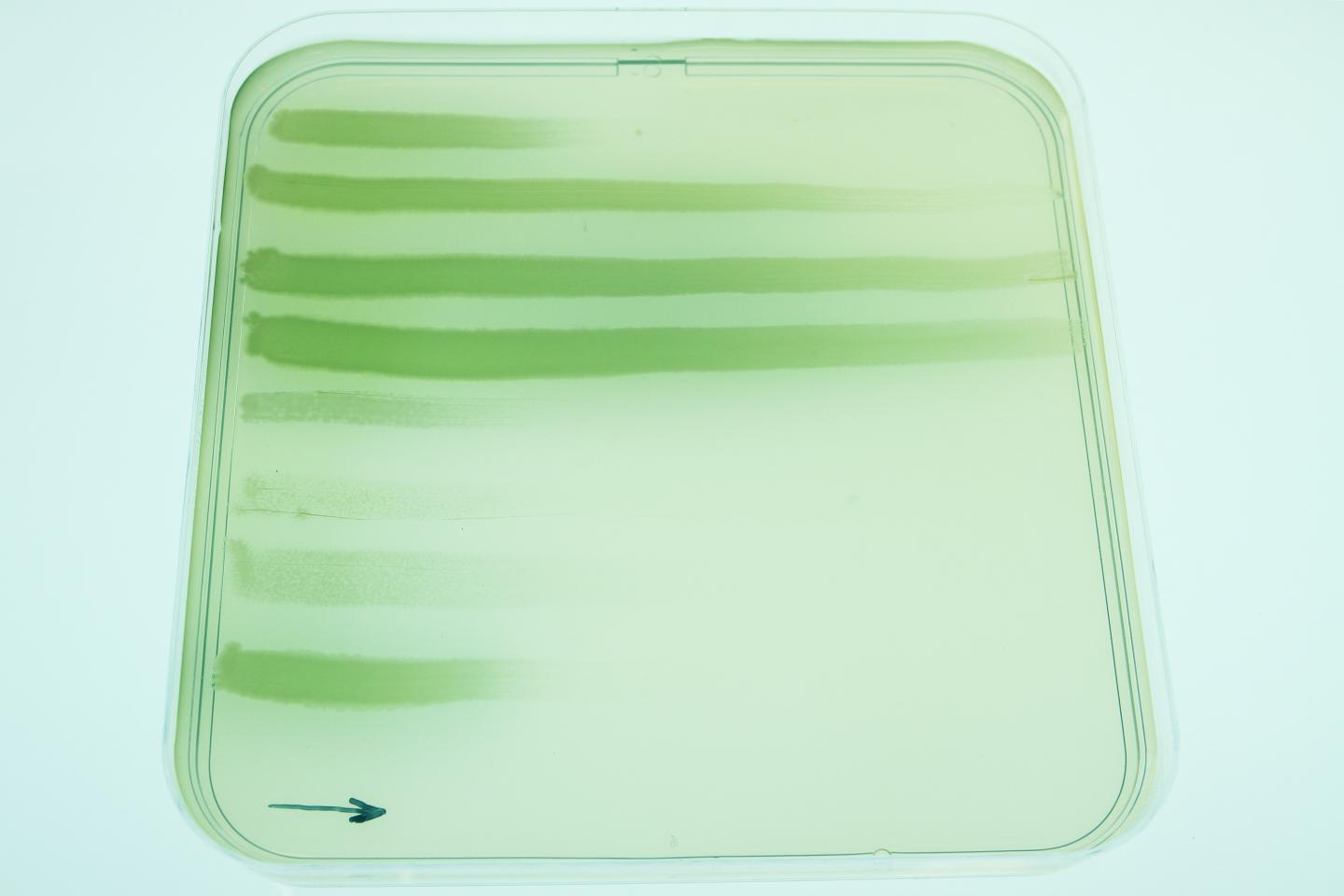
From their experiments, the researchers found that P. aeruginosa produces some quite different distinct cases of evolved collateral sensitivities when responding to different drugs. Some of these were found to remain stable over time which either led to an increased extinction or just a complete absence of the multidrug resistance evolution. They also found that the way in which the effectiveness of the drugs was determined was by looking at the order in which they were used, the ingrained genetic mechanisms and the evolutionary sacrifices the bacteria undergo while evolving antibiotic resistance.
In this particular instance, the bacteria were unable to adapt when faced with the administration of antibiotics and soon became extinct. “The effects of changing certain drug classes and the impact of evolutionary costs on the development of resistance demonstrate the enormous potential of evolutionary principles for the design of new, sustainable antibiotic therapies,” comments senior author Hinrich Schulenburg, Professor in Zoology at the KEC. The next step for the professor and his colleagues is to further develop these strategies so that in the future, they could potentially be used inpatient treatment.

