While the organ transplant research and technology is consistently improving, organ rejection, both in the long and short term, continues to be a risk for the 25,000 transplants that occur in the U.S. each year. But help may be on its way thanks to research from Yale. Scientists there have created a way to mask the foreign body of the donor organ from the host’ immune system with the use of a new nanoparticle drug conveyance method.
One of the leading causes of organ rejection is the reaction of effector memory T-cells, a specific type of powerful white blood cells, to the donor organ, especially in the cases where the organ originates from a deceased donor. Organs from deceased donors suffer from damage and can take weeks to recover after transplantation. However, the current method of treating organ rejection, a dose of small interfering RNA, only lasts a few days in the body, not long enough to ensure the health of both organ and recipient.
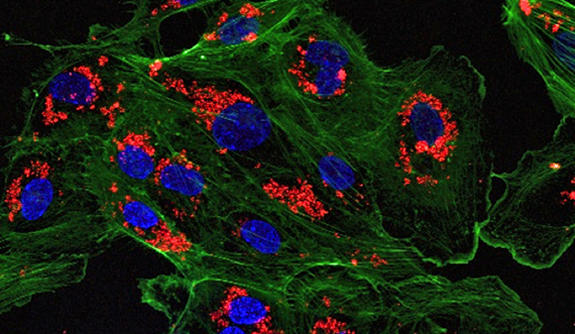
Small interfering RNA, or siRNA, works by blocking the expression of the genes which activate the effector memory T-cells. The key area that the *siRNA needs to operate is in the endothelial cells of blood vessel associated with the donor organ, but the conventional delivery system spread siRNA throughout the recipient’s body leading side effects on the endothelial cells of all organs.
The new method from Yale relies on a type of special type of nanoparticle device. The device is composed polymer based nanoparticle and has a small positive charge specifically to pair with siRNA’s negative charge, which allows it to hold more than typical a nanoparticle device. *siRNA delivery using this device allows for a slow release over time direct to the donated organ, avoiding side effects to other organs.
The device and delivery method were tested on a human artery transplanted to a mouse. The nanoparticles were delivered to the artery before the transplant, and the siRNA was found to be present and active six weeks later, with no *siRNA found in the endothelial cells of mouse’s native organs. The full study and findings are available in Nature Communications.
Researchers will next test their nanoparticles with a technique, developed at Cambridge University, called ex vivo normothermic machine perfusion. Used in kidney transplant, the donated organ is filled with oxygen loaded, heated red blood cells before the transplant procedure, to help heal natural damage from deceased donors. The hope is that adding the nanoparticles with *siRNA at this point will make a controlled and direct delivery where it can be most efficient and further minimize the possibility of other organ damage as well as rejection.
*Small interfering RNA (siRNA), sometimes known as short interfering RNA or silencing RNA, is a class of double-stranded RNA molecules, 20-25 base pairs in length, similar to miRNA, and operating within the RNA interference (RNAi) pathway. It interferes with the expression of specific genes with complementary nucleotide sequences by degrading mRNA after transcription, resulting in no translation. Source: Wikipedia
More News to Read
- Does Physical Activity Affect the Brain’s Aging Process?
- Gaining a Deeper Understanding of the Relationship Between DNA and Cell Function
- Can This New Heart Model Save Muscles During Heart Attack?
- Harvard’s New Exosuit Will Push the Limits of Human Performance
- The New Cheap and Fast Way to Make Supercapacitor Electrodes For Electric Cars











