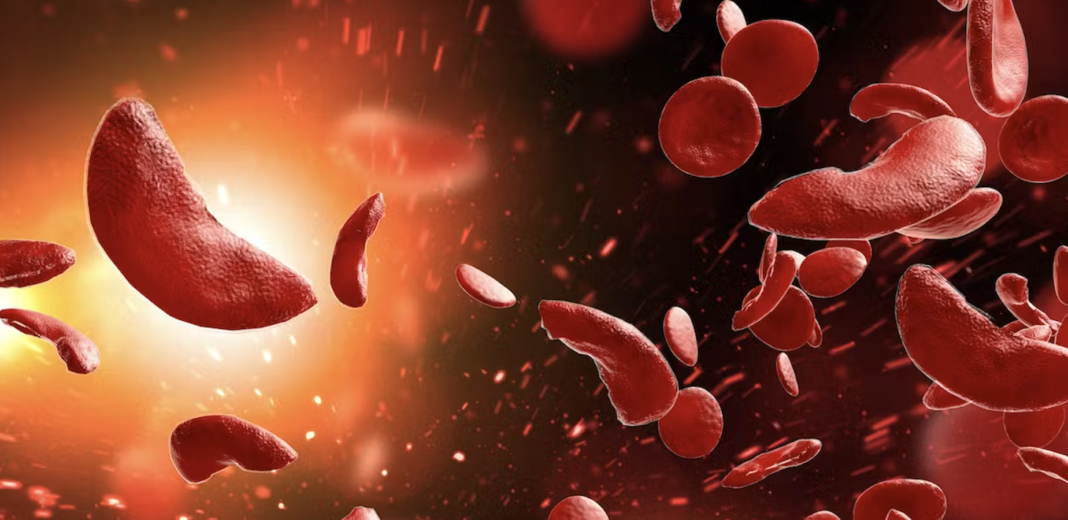
Sickle Cell Disease (SCD) and Beta Thalassemia are widespread blood disorders that pose significant health risks to millions of individuals worldwide. In recent research conducted by scientists at St. Jude Children’s Research Hospital and the Broad Institute of MIT and Harvard, a revolutionary gene editing technology called adenosine base editing has shown remarkable potential in the treatment of these life-threatening anemias. This blog post delves into the groundbreaking study published in Nature Genetics, highlighting the superiority of base editing in reinstating fetal hemoglobin expression when compared to other genome editing techniques.
The Challenge of Hemoglobin Disorders: SCD and Beta Thalassemia result from genetic mutations affecting the gene responsible for producing adult hemoglobin. These mutations lead to defective hemoglobin, causing severe complications. However, an alternative subunit of hemoglobin, known as fetal hemoglobin, has shown therapeutic benefits when expressed in patients with these disorders. The goal of this research was to identify and optimize a genomic technology capable of editing the fetal hemoglobin gene.
The Promise of Base Editing: In their study, the research team employed adenosine base editing, a next-generation genome editing technology. Unlike the widely known CRISPR/Cas9 system, which introduces double-stranded breaks and potential unwanted consequences, base editing allows for precise alterations of the DNA sequence. By leveraging base editing, the scientists successfully increased the expression of fetal hemoglobin, surpassing other genome editing techniques in terms of stability, uniformity, and overall effectiveness.
Advantages of Fetal Hemoglobin Expression: Fetal hemoglobin plays a crucial role in countering the adverse effects of SCD and Beta Thalassemia. During fetal development, gamma-globin, a subunit of hemoglobin, combines with alpha-globin to form fetal hemoglobin. However, shortly after birth, gamma-globin expression is naturally switched off, giving way to adult hemoglobin production. The ability to reactivate gamma-globin expression postnatally through base editing offers a potential “one-size-fits-all” treatment approach for patients with various causative mutations, providing a universal therapeutic solution.
Comparing Editing Technologies: The research team meticulously examined the outcomes of different genome editing approaches on the DNA sequence of the target genes. They found that base editing yielded significantly more homogeneous results compared to nucleases like CRISPR/Cas9, which produced complex mixtures of various DNA sequence outcomes. Moreover, base editing achieved higher levels of fetal hemoglobin expression, making it a more potent and precise editing method for therapeutic purposes.
Addressing Safety Concerns: While base editing exhibited superior efficacy, safety remains a paramount concern. The study noted that base editing caused fewer genotoxic events and undesired mutations compared to conventional Cas9 nucleases. However, the researchers acknowledged the need for extensive safety testing and optimization before implementing base editing as a clinical therapy. Though the study demonstrated minimal undesired changes, thorough investigation and risk evaluation are essential.
The Road to Broadly Available Cures: The findings of this study open up new possibilities in the field of gene editing therapeutics for SCD and Beta Thalassemia. By comparing Cas9 nucleases and base editing approaches, researchers strive to identify the most effective strategies for combating these blood disorders. Clinical trials are currently underway to evaluate the potential of base editing and different Cas9 nuclease approaches, with St. Jude participating actively. These advancements bring us closer to the ultimate goal of developing widely accessible and effective cures.
The revolutionary adenosine base editing technology presents a significant breakthrough in the treatment of SCD and Beta Thalassemia. By successfully restoring fetal hemoglobin expression through precise DNA alterations
What is gene therapy and how is it done? Gene therapy is an innovative medical approach that aims to treat or prevent diseases by modifying an individual’s genetic material. It involves introducing healthy genes into the patient’s cells to replace or supplement the faulty genes causing the disease. This can be accomplished through different methods, including viral vectors that deliver the therapeutic genes into target cells or genome editing techniques like CRISPR-Cas9, which directly modify the patient’s DNA.
What is an example of gene therapy? One notable example of gene therapy is the treatment of severe combined immunodeficiency (SCID), also known as “bubble boy” disease. In this condition, patients have a deficient immune system, making them highly susceptible to infections. Gene therapy has been used to successfully treat SCID by introducing a functional copy of the faulty gene responsible for the immune deficiency. This enables the patient’s cells to produce the necessary proteins and restore immune function.
What is gene therapy in simple terms? Gene therapy can be understood as a medical technique that uses genetic modifications to treat or prevent diseases. By introducing healthy genes or altering faulty ones, gene therapy aims to correct the underlying genetic abnormalities causing the disease. This innovative approach holds the potential to provide long-lasting or even permanent solutions for various genetic disorders and other illnesses with a genetic component.
Why is gene therapy not widely successful? While gene therapy shows great promise, it has faced challenges that have hindered its widespread success. Some factors contributing to its limited success include:
- Delivery hurdles: Efficiently delivering therapeutic genes to target cells in the body can be challenging. Ensuring proper delivery and integration of the genes into the patient’s cells remains a significant obstacle.
- Immune response: The immune system may recognize the viral vectors used in gene therapy as foreign invaders, leading to immune reactions that reduce the effectiveness of treatment.
- Off-target effects: Gene editing techniques, such as CRISPR-Cas9, can have unintended modifications in the genome, potentially causing unpredictable and unwanted consequences. Ensuring precision and minimizing off-target effects is crucial for the success of gene therapy.
- Complexity of genetic diseases: Many diseases have complex genetic causes involving multiple genes and interactions. Addressing such complexities with gene therapy poses significant scientific and technical challenges.