A new technique carried out by a group of several Yale researchers has for the first time ever, managed to use gene editing to correct a mutation within a fetus that causes a certain kind of anemia. It was described in a recent paper published in the journal Nature Communications.
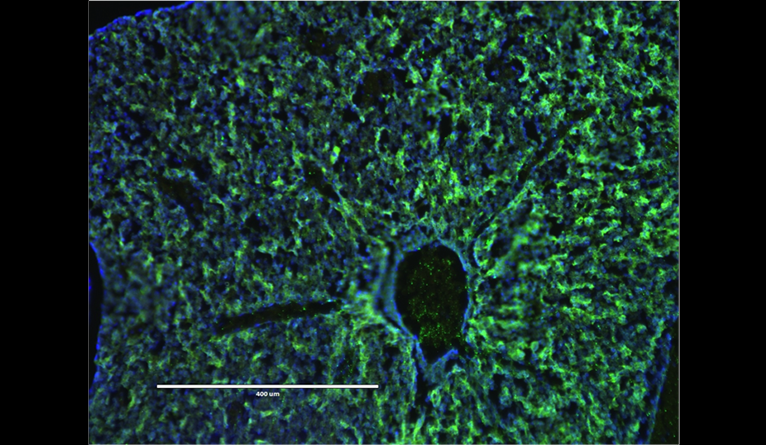
The technique involves injecting a mix of nanoparticles containing both donor DNA and peptide nucleic acids (PNAs). PNAs are synthetic molecules that mimic DNA. Binding to their target gene they form a triple helix, which is used to repair the mutation. In this particular study, the nanoparticles were injected into the mice fetuses. Results showed that at just four months after birth, the mice were cured of thalassemia, an inherited blood disorder.
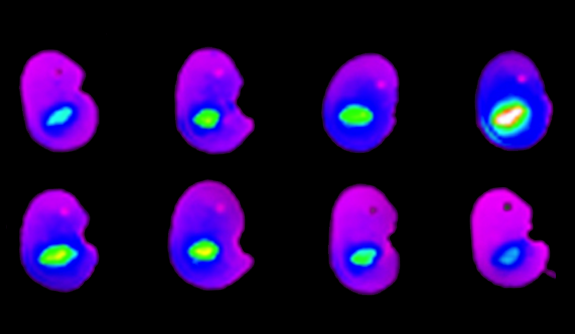
Peter M. Glazer, MD, professor of therapeutic radiology and of genetics, is the man responsible for developing the technique which sees PNA and DNA combine in order to repair gene mutations. Here’s what he had to say on the breakthrough: “The treated mice had normal blood counts, their spleens returned to normal size, and they lived a normal lifespan – whereas, the untreated ones died much earlier. So, we have a long-term survival benefit, which is pretty dramatic.”
The researchers say that using nanoparticles to deliver the PNAs is essential. When injected intravenously on its own, PNAs take just 30 minutes or so to clear from circulation. When injected with nanoparticles they are present for far longer. The man responsible for making the nanoparticles is Mark Saltzman, Yale’s Goizueta Foundation Professor of Biomedical Engineering, Chemical and Environmental Engineering, and professor of physiology. He designed them using a degradable polymer and made so small that they could easily accumulate in the liver of the fetus.
“People who have thalassemia, they get sicker and sicker as they go on because they don’t have normal red blood cell function, and it gets harder to treat,” says Saltzman. “Here, we’re correcting the gene very early in development, so you see more benefits because they don’t get sick.” While most other gene-editing procedures are limited to working with cells in a petri dish, this technique uses live animals in which to get results, making it more precise.
One of the main challenges of this study was making sure the therapy worked after just one injection as multiple injections increase the risk of harm to the fetus. This is where David H. Stitelman, MD, came in very useful as an assistant professor of pediatric surgery with an expertise in the accessing of fetal stem cells. “You have to catch these cells while they are in a state of massive proliferation, so this is literally a once-in-a-lifetime opportunity,” he says.
The team is now in the process of seeing how their technique can be used to treat other genetic, single-gene disorders including sickle cell and cystic fibrosis. “If a baby could be born with a lower burden of disease – or no disease whatsoever – that would have a profound impact on that child’s life as well as the family,” says the study’s first author, Adele Ricciardi, a current MD/ Ph.D. student. The number of people this could help is enormous. Now that scientists know it’s possible, they just need to make it happen.
More News to Read
- UCLA Scientists Report Their Deepest Understanding Yet of the Enzyme Telomerase
- The World’s Most Sensitive Experiment for Dark Matter is Now Underway
- On the Hunt for Clandestine Nuclear Weapon Sites
- Without Teamwork, There will be No Colonizing on Mars
- Engineers Develop A New Cloaking Material That Can Hide Hot Objects