Blindness is a condition that affects millions of people across the globe. While some people only suffer partial blindness, some are left completely without sight. Sometimes people are born with no sight and other times it occurs gradually. Either way, it’s not a nice condition and one that scientists have battled with for a long time to try and find some kind of cure or effective form of treatment. But so far, nothing seems to be that effective.
However, that may be about to change with thanks to two research teams from Stanford. One of the devices they’ve come up with is a bionic vision system that’s based on photovoltaic implants and is currently waiting to be approved to used in Europe as a trial. Another system they’ve designed could be ready to test in animals within the next five years and that’s based on vitro studies of the retina. Both are intended to give those suffering with progressive diseases of the retina a chance to regain some sight.
Retinitis pigmentosa is the number one cause of inherited blindness and affects as many as 1 in every 4,000 in the United States alone. Most people with the disease suffer a loss of night vision in childhood, to begin with. It will then progress to affect peripheral and central vision too, leaving people unable to carry out their daily routine tasks as they normally would. Macular degeneration is a condition that usually affects older persons and is the leading cause of vision loss in the United States for those aged over 60. It gradually destroys light-sensitive cells in the retina’s center.
Chip Goehring is president of the American Macular Degeneration Foundation and he says, “Many of these folks are going to be losing their central vision so it’s absolutely vital that we have options for the restoration of sight, including biological and mechanical approaches – stem cell therapies for photoreceptor replacement, gene therapies to restore dysfunctional retinal tissues, and prosthetic retinas that can serve an even wider population of people with vision loss.”
In patients with retinal diseases the rods and cones that resemble light-sensitive cells break down and so far scientists haven’t been able to figure out how to stop or even slow this process. One good thing about both retinitis pigmentosa and macular degeneration is that they spare some of their ganglion and bipolar cells which are great news as this means scientists can use mini-electrodes to artificially stimulate the patient’s neurons.
Daniel Palanker, Ph.D., and professor of ophthalmology at Stanford has developed various devices over the years to help diagnose and treat eye disease. One of the devices is a neuro stimulator for enhancing tear secretion in those suffering from dry eye syndrome. Another is a patterned laser scanning photocoagulator that’s used in treating multiple retinal disorders without damaging the delicate tissue surrounding the spots.
Spread across various parts of the world are around 20 different research groups, each working on bionic visions systems. But so far only one retinal prosthesis has been approved to be used in the United States, and that’s called the ARGUS II. It was developed by scientists at USC and Second Sight Medical Products Inc and is currently being used by around 200 patients worldwide. The system itself comprises of a tiny video camera that’s mounted on a pair of goggles, a small video processing unit, a transmitting antenna, a receiving antenna, and a 60-electrode array. Those that use the system have reported being able to see broad patterns of light. such as doorways.
A newer implant system called Alpha-IMS from Retina Implant AG has been used in a few patients in Europe. The difference with this implant is that it’s placed under the retina and is powered by a cable that runs from the eye to a receiver that’s implanted behind the ear. Patients using this device have reported being able to see ghostly shapes of objects such as bananas or apples on a table nearby.
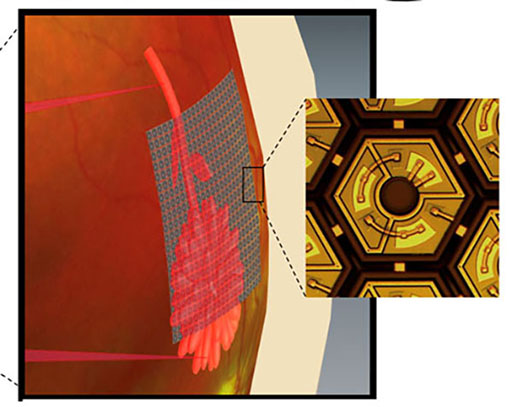
The new prosthetic device in which Palanker’s just designed is called PRIMA. It’s similar to ARGUS II in that it features a tiny camera mounted on top of some goggles. However, with this device, there are no bulky cables or antennas to worry about. It simply relies on arrays of photo bodies containing hundreds of pixels working like solar panels. Surgeons then arrange these chips, like tiles, to replace the light-sensitive rods and cones that are causing the problems in the central retina. The display is illuminated by powerful pulses of near-infrared light when PRIMA’s camera captures an image.
In order to sufficiently test the system, the researchers implanted PRIMA chips into rodents before exposing them to flashes of light or flickering computer screens. Their visual activity was then measured. “It turned out that the prosthetic acuity exactly matched the 70-micron resolution of the implant, which is half the acuity of the rats’ natural vision,” said Palanker. “Since stimulation thresholds were much lower than the safety limits, we decided to develop even smaller pixels to enable better vision. More recent behavioral tests, conducted by the French collaborators in primates, have confirmed our results with rodents.”
Until the human trials are completed, we won’t really know the full effect of the implant. However, Palanker is hopeful they can achieve at least a 20/250 vision with 70-micron pixels. Although that doesn’t sound much when considering the legal standard for blindness is 20/200, it may still be enough for some to read very large print or see the face of a loved one. For the next version of the device, Palanker says, “We should be able to put more than 12,000 pixels within 15 degrees of the visual field.”
But E.J. Chichilnisky, Ph.D., a Stanford professor of neurosurgery and of Ophthalmology wants more than that. His goal is to build a visual prosthesis that’s so powerful it can stimulate specific neurons found within the retina, opposed to a general area. As part of his research, Chichilnisky and colleagues used eye tissue samples that have been taken from primates and expose them to various patterns of light while mounted atop the microchip arrays. In doing this they’ve been able to gain a deeper understanding of the electrical responses of five different types of retinal ganglion cells which make up 75 percent of the visual signals that are sent to the brain. They’ve also learned how to replicate those patterns, artificially stimulating the ganglion cells as a result.
Learning how to replicate these signals gets the team one step closer to achieving the ultimate goal of developing a high-acuity visual prosthesis that signals the retina’s neurons to fire just right. Chichilnisky and Palanker often discuss their research informally together as their offices are so close to one another and they can easily benefit from the other’s input. Both are confident that their work may someday help much more people suffering from blindness.
More News to Read
- New Hydrogel Material Could Help Tissue Repair After Stroke
- New Bacterium Discovered That Can Nucleate Ice
- Does the Answer to Better Patient Care Lie in Machine Learning?
- MAG-LEV Audio: Futuristic Technology Meets an old Format
- New Grant Allocated to Imperial College Professor to Research Incurable Lung Disease

